Visiting a podiatrist, a medical professional specializing in diagnosing and treating conditions of the foot, ankle, and related structures, is crucial for maintaining foot health and overall well-being. Here are some specific situations when you should consider seeing a podiatrist:
1. Persistent Foot or Ankle Pain
- Symptoms: Continuous pain in your feet or ankles that doesn’t improve with rest or over-the-counter pain medication.
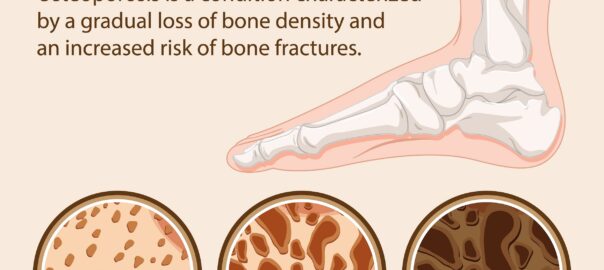
- Potential Issues: Conditions such as arthritis, plantar fasciitis, tendonitis, or stress fractures.
2. Heel Pain
- Symptoms: Sharp pain in the heel, especially first thing in the morning or after standing for long periods.
- Potential Issues: Plantar fasciitis, heel spurs, or Achilles tendonitis.
3. Foot Deformities
- Symptoms: Visible deformities such as bunions, hammertoes, or high arches.
- Potential Issues: Structural abnormalities that can worsen over time and affect mobility.
4. Numbness, Tingling, or Burning Sensations
- Symptoms: Unexplained numbness, tingling, or burning in the feet.
- Potential Issues: Nerve problems like peripheral neuropathy or tarsal tunnel syndrome.
5. Changes in Skin or Nails
- Symptoms: Discoloration, thickening, or ingrown nails; blisters, sores, or warts on your feet.
- Potential Issues: Fungal infections, bacterial infections, warts, or skin cancers.
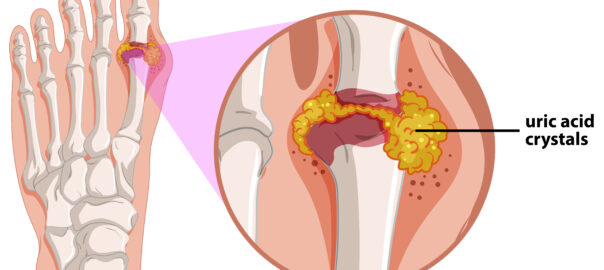
6. Swelling or Redness
- Symptoms: Persistent swelling, redness, or warmth in the feet or ankles.
- Potential Issues: Infections, gout, or deep vein thrombosis (DVT).
7. Diabetes Management
- Symptoms: Routine care for those with diabetes, even without foot problems.
- Potential Issues: High risk of foot complications such as ulcers, infections, and neuropathy.
8. Injuries
- Symptoms: Sprains, fractures, or wounds that are not healing.
- Potential Issues: Proper diagnosis and treatment to ensure correct healing and prevent long-term damage.
9. Difficulty Walking
- Symptoms: Changes in the way you walk, such as limping or favoring one foot.
- Potential Issues: Musculoskeletal issues that need to be addressed to improve mobility.
10. Athletic Injuries and Performance Issues
- Symptoms: Recurring injuries or pain associated with physical activities.
- Potential Issues: Overuse injuries, improper footwear, or gait abnormalities.
Preventive Care
Even if you don’t have specific symptoms, it can be beneficial to see a podiatrist for preventive care, especially if you have risk factors such as a family history of foot problems, a job that requires standing for long periods, or participation in high-impact sports.
Regular visits to a podiatrist can help maintain foot health, detect potential problems early, and provide appropriate treatment to avoid complications.podiatrist