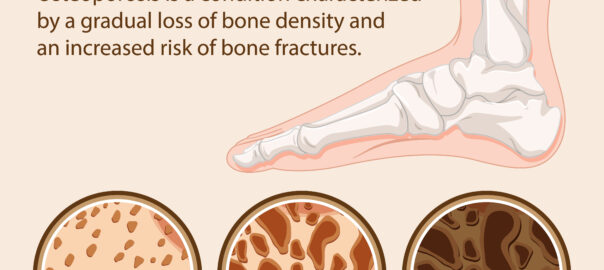
Flat feet, also known as fallen arches, is a condition where the arches on the inside of your feet are flattened, causing the entire sole of your foot to touch the floor when you stand. It’s a common condition that can be present at birth or develop over time due to factors like age, injury, or wear and tear on the feet.
Some people with flat feet may not experience any pain or discomfort, while others may have symptoms such as:
- Pain or achiness in the feet, especially in the arch or heel area.
- Swelling along the inside of the ankle.
- Difficulty standing for long periods.
- Foot movement issues or feeling like the feet tire easily.
If you suspect you have flat feet and it’s causing you discomfort, it’s a good idea to see a doctor or a podiatrist (foot specialist). They can examine your feet, assess your symptoms, and recommend appropriate treatments. Treatment options may include:
- Orthotic devices: Custom-made shoe inserts (orthotics) can provide support and alleviate discomfort by redistributing pressure on the foot.
- Supportive footwear: Shoes with good arch support and stability can help reduce pain and provide better alignment.
- Physical therapy: Specific exercises and stretches can strengthen muscles and improve foot function.
- Over-the-counter arch supports: These can offer relief for mild cases.
- In severe cases: Surgery might be considered, but this is typically rare and only for extreme cases where other treatments haven’t been effective.
Remember, having flat feet doesn’t necessarily mean you’ll have problems. Many people with flat feet don’t experience any symptoms or issues and lead perfectly normal, pain-free lives. But if you’re experiencing discomfort or pain, it’s essential to seek professional advice to explore the best options for managing your condition.